Abstract
Background: CPX-351 is a liposomal encapsulation of cytarabine and daunorubicin maintained at a synergistic 5:1 molar ratio. It is approved for the treatment of patients with newly diagnosed therapy related myeloid leukemia (t-AML) or with AML with myelodysplasia-related changes (AML-MRC). Improved outcomes with CPX-351 compared to 7+3 have been reported irrespective of AML subtype (t-AML, AML-MRC), age subgroup (60 to 69 vs 70 to 75 years), prior hypomethylating agent (HMA) exposure and whether the patients undergo transplant. Here we compare outcomes of patients with de-novo AML vs those with secondary AML when treated with CPX-351.
Methods: We retrospectively identified all previously untreated AML patients who received CPX-351 as first line therapy at Moffitt Cancer Center between August 2017 and July 2020. Charts were reviewed to collect demographic data, disease characteristics and outcomes. Overall survival was calculated from date of diagnosis.
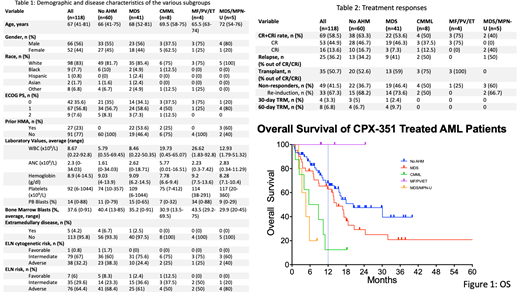
Results: A total of 118 patients were identified. The median age at diagnosis was 67 years (range 41-81 years). 66% patients were male (n=66). We reviewed prior history of antecedent hematologic malignancy (AHM) and divided patients into 5 cohorts: (A) No prior AHM (n=60), (B) Prior history of MDS (n=41), (C) prior history of chronic myelomonocytic leukemia (CMML) (n=8), (D) prior history of myeloproliferative neoplasm (MPN) including myelofibrosis, polycythemia vera and essential thrombocytosis (MF/PV/ET; n=4) and (E) prior myelodysplastic syndrome/myeloproliferative neoplasm-unclassifiable (MDS/MPN-U) (n=5). Table 1 shows baseline disease characteristics of all cohorts.
Complete remission plus complete remission with incomplete hematologic recovery (CR+CRi) rate for the entire cohort was 58.5% (n=69). Of all patients who achieved CR/CRi, 36.2% (n=25) ultimately relapsed. 50.7% (n=35) patients proceeded to an allogeneic stem cell transplant in CR1. Of the 49 non-responding patients (41.5%), 33 (67.3%) were re-induced with a high dose cytarabine based regimen. The CR/CRi rate after re-induction was 57.5% (n=19). At a median follow up of 15 months the median duration of remission for the entire cohort was 29 months (mos). The duration of remission was significantly different for the 5 cohorts (A: 29 mos, B: not reached, C: 8 mos, D: not reached, E: 2.5 mos, p=0.0061). The 30 day treatment related mortality for the entire group was 3.3% (n=4).
At a median follow up of 18.1 mos for all 118 patients, the median overall survival is 17.3 mos. Median OS for cohort A is 20.4 mos, cohort B is 14.8 mos, cohort C 7.2 mos, cohort D is not reached and cohort E is 4.6 mos (p 0.002). Patients without an AHM had an improved OS compared to those with pre-existing CMML (20.4 vs 7.2 mos; p 0.0027) or MDS/MPN-U (20.4 vs 4.6 mos; p 0.004). However, absence of AHM was not associated with statistically significant longer OS compared to patients with prior MDS (20.4 vs 14.8 mos; p 0.1224). When looking at the impact of prior hypomethylating agent (HMA) therapy in cohort B, there was a significant OS advantage for patients who were not treated with HMA for prior MDS compared to those who were (25 vs 13 mos; p 0.0061). On the contrary, for patients with CMML (cohort C) treated with prior HMA, this had no impact on OS after CPX-351 induction (8 months vs 8 months; p=0.9506).
We then looked at the pre and post next generation sequencing (NGS) data for the patients that achieved CR/CRi with CPX-351. From the 52 patients that had mutations on NGS at diagnosis, 19 (36.5%) patients cleared mutations and 33 (63.5%) did not clear mutations. From the 36 patients that had secondary MDS like mutations on diagnosis, 15 (41.7%) patients cleared the mutations while 21 (58.3%) did not. For both of these cohorts of patients the OS and rate of relapse was not different. However, RFS was better for patients that cleared mutations, but this did not reach statistical significance (27 vs 11 mos, p=0.2738).
Conclusion: Overall survival of patients treated with CPX-351 for AML with no known AHM was significantly greater compared to patients with prior history of CMML or MDS/MPN-U. However, a prior history of MDS did not lead to statistically significant decrease in OS. Prior HMA exposure results in inferior outcomes in patients with prior MDS, but not CMML, likely because of the shorter OS for the entire CMML cohort overall. Pre and post NGS data showed that clearing mutations at remission did not affect OS and rate of relapse.
Sallman: Shattuck Labs: Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Syndax: Membership on an entity's Board of Directors or advisory committees; Aprea: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Consultancy; Kite: Membership on an entity's Board of Directors or advisory committees; Magenta: Consultancy; Incyte: Speakers Bureau; Intellia: Membership on an entity's Board of Directors or advisory committees; Agios: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Komrokji: Acceleron: Consultancy; Geron: Consultancy; Jazz: Consultancy, Speakers Bureau; PharmaEssentia: Membership on an entity's Board of Directors or advisory committees; AbbVie: Consultancy; Taiho Oncology: Membership on an entity's Board of Directors or advisory committees; BMSCelgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Padron: Taiho: Honoraria; Kura: Research Funding; Incyte: Research Funding; Blueprint: Honoraria; Stemline: Honoraria; BMS: Research Funding. Kuykendall: Protagonist: Consultancy, Research Funding; Novartis: Honoraria, Speakers Bureau; Celgene/BMS: Honoraria; Blueprint: Honoraria; Abbvie: Honoraria; Pharmaessentia: Honoraria; Incyte: Consultancy. Lancet: AbbVie: Consultancy; Daiichi Sankyo: Consultancy; ElevateBio Management: Consultancy; Millenium Pharma/Takeda: Consultancy; Agios: Consultancy; Astellas: Consultancy; Celgene/BMS: Consultancy; BerGenBio: Consultancy; Jazz: Consultancy. Sweet: Gilead: Membership on an entity's Board of Directors or advisory committees; AROG: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Astellas: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol Meyers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal